Study in China reveals tumor Treg specific epigenetic regulation mechanism and targeting strategy
Source:Xiaoming Wang
2024-02-28
Treg cells, which are essential for maintaining immune tolerance and preventing autoimmune diseases, also infiltrate into tumor tissues and suppress anti-tumor immunity. Targeting Treg cells could improve the immune suppressive tumor microenvironment (TME) and elicit effective anti-tumor immunity. However, systemic depletion of Treg cells would disturb the immune homeostasis and thereby lead to deleterious autoimmune complications. Therefore, it is important to identify the specific regulatory molecules that could be used to selectively target intratumoral Treg cells without affecting systemic or peripheral Treg cells.
On February 14, 2024, a research article titled “Targeting JMJD1C to selectively disrupt tumor Treg fitness enhances anti-tumor immunity” in Nature Immunology by the teams led by Drs. Xiaoming Wang (School of Basic Medical Sciences, Nanjing Medical University), Jun Qin (Shanghai Institute of Nutrition and Health, Chinese Academy of Sciences) and Mingyue Zheng (Shanghai Institute of Materia Medica, Chinese Academy of Sciences). The study reported that tumor Treg displayed distinct epigenetic status from peripheral Treg and the authors identified the tumor Treg specific epigenetic regulator: H3K9me2 demethylase JMJD1C, which is gradually upregulated along the course of Treg fitting into TME and essential for tumor Treg fitness, whereas not required for peripheral Treg. Mechanistically, on the one side, Jmjd1c facilitates NRP1 and PD1 expression to repress AKT signal and IFNg production as a H3K9me2 demethylase; on the other side, JMJD1C also directly demethylases STAT3 to prevent IFNg expression in tumor Treg. IFNg ablation rescued the adverse effect of JMJD1C loss on tumor Treg. Importantly, utilizing a deep learning-based virtual screening, the authors developed an oral administration inhibitor of JMJD1C, which showed similar tumor growth inhibition effect as Jmjd1c knockout by acting through JMJD1C expressed in tumor Treg without evidence of toxicity.
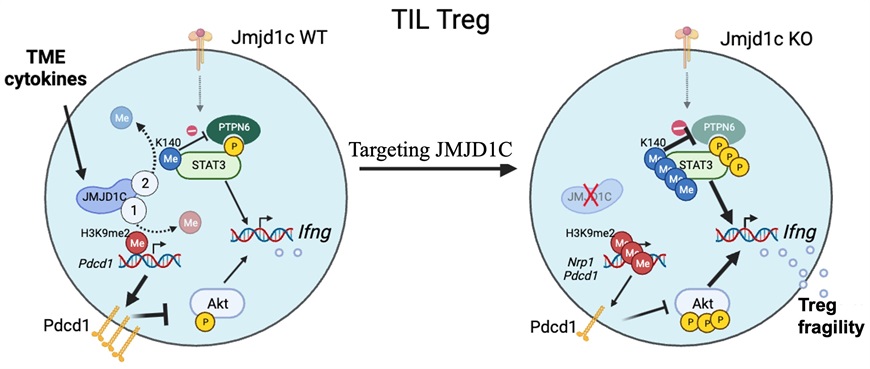
The study revealed JMJD1C as a tumor Treg specific epigenetic regulator which could be used for selective targeting of tumor Treg. JMJD1C deletion had no impact on peripheral Treg and autoimmune disease progress, but disrupted tumor Treg fitness and dramatically boosted anti-cancer T cell response. Therefore, the study provided a potential Treg-based tumor immunotherapy strategy and also generated a small compound with high efficacy.
The work was funded by grants from the National Natural Science Foundation of China, National Key R&D Program of China and etc.
Links: https://www.nature.com/articles/s41590-024-01746-8
On February 14, 2024, a research article titled “Targeting JMJD1C to selectively disrupt tumor Treg fitness enhances anti-tumor immunity” in Nature Immunology by the teams led by Drs. Xiaoming Wang (School of Basic Medical Sciences, Nanjing Medical University), Jun Qin (Shanghai Institute of Nutrition and Health, Chinese Academy of Sciences) and Mingyue Zheng (Shanghai Institute of Materia Medica, Chinese Academy of Sciences). The study reported that tumor Treg displayed distinct epigenetic status from peripheral Treg and the authors identified the tumor Treg specific epigenetic regulator: H3K9me2 demethylase JMJD1C, which is gradually upregulated along the course of Treg fitting into TME and essential for tumor Treg fitness, whereas not required for peripheral Treg. Mechanistically, on the one side, Jmjd1c facilitates NRP1 and PD1 expression to repress AKT signal and IFNg production as a H3K9me2 demethylase; on the other side, JMJD1C also directly demethylases STAT3 to prevent IFNg expression in tumor Treg. IFNg ablation rescued the adverse effect of JMJD1C loss on tumor Treg. Importantly, utilizing a deep learning-based virtual screening, the authors developed an oral administration inhibitor of JMJD1C, which showed similar tumor growth inhibition effect as Jmjd1c knockout by acting through JMJD1C expressed in tumor Treg without evidence of toxicity.
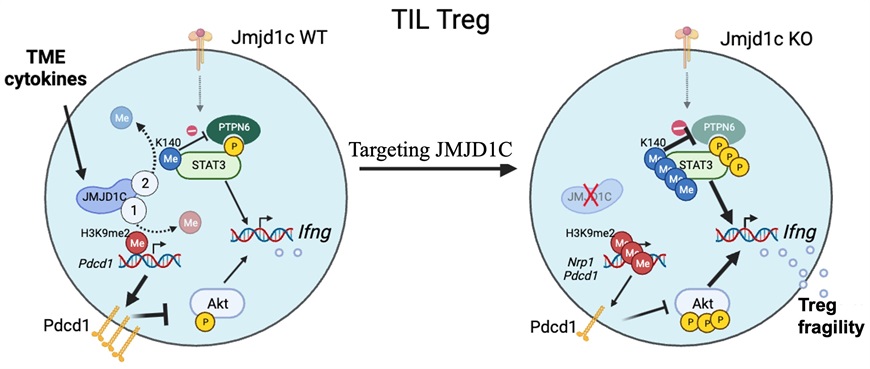
The study revealed JMJD1C as a tumor Treg specific epigenetic regulator which could be used for selective targeting of tumor Treg. JMJD1C deletion had no impact on peripheral Treg and autoimmune disease progress, but disrupted tumor Treg fitness and dramatically boosted anti-cancer T cell response. Therefore, the study provided a potential Treg-based tumor immunotherapy strategy and also generated a small compound with high efficacy.
The work was funded by grants from the National Natural Science Foundation of China, National Key R&D Program of China and etc.
Links: https://www.nature.com/articles/s41590-024-01746-8